Prostate Cancer
- font size decrease font size increase font size
 The prostate is a glandular organ that is normally about 3 cm long (slightly more than 1 inch) and lies at the neck of the bladder and in front of the rectum. The prostate produces a thin, milky fluid that is added to the sperm at the time of ejaculation. It surrounds the urethra, which is a tubular structure that carries sperm and urine out of the penis, therefore prostate diseases often affect urination, ejaculation, and rarely defecation.
The prostate is a glandular organ that is normally about 3 cm long (slightly more than 1 inch) and lies at the neck of the bladder and in front of the rectum. The prostate produces a thin, milky fluid that is added to the sperm at the time of ejaculation. It surrounds the urethra, which is a tubular structure that carries sperm and urine out of the penis, therefore prostate diseases often affect urination, ejaculation, and rarely defecation.
Prostate cancer is the most common cancer in men, no matter your race or ethnicity. More than 80% of prostate cancers are diagnosed in men older than 65 years of age. Due to this fact most countries recommend yearly screening for men above the age of 40. Almost all prostate cancers arise from the secretory glandular cells in the prostate. Therefore, almost all prostatic cancers are prostatic adenocarcinomas. Other types of cancers are transitional cell and squamous cell.
Prostate Cancer Causes
The cause of prostate cancer is unknown, but hormonal, genetic, environmental, and dietary factors are thought to play roles. The following risk factors have been linked with development of this condition:
• Age: There is a strong correlation between increasing age and developing prostate cancer. The incidence of prostate cancer increases steadily from fewer than 1 in 100,000 for men 40 years of age to 1,146 per 100,000 in men 85 years of age. The median age at diagnosis of prostate cancer is 70.5 years of age. Autopsy records indicate that 70% of men older than 90 years of age have at least one region of cancer in their prostate. Therefore more than 2/3 of the aged people have cancer of the prostate though most die from other causes related to old age i.e heart diseases.
• Race: African American men are 1.6 times more likely than white men to develop prostate cancer. They are also 2.4 times more likely to die from their disease as compared to white men of a similar age. Although, these racial criteria have been used to study and describe the disease in the past, there is no defined biologic basis for this classification. In other words, these differences in diagnosis and death rates are more likely to reflect a difference in factors like environmental exposure, diet, lifestyle, and health-seeking behavior rather than any racial susceptibility to prostate cancer. Recent evidence, however, suggests that this disparity is progressively decreasing with high chances of complete cure in men undergoing treatment for organ-confined prostate cancer (cancer that is limited to within the prostate without spread outside the confines of the prostate gland) irrespective of race.
• Genetic factors: Men who have a history of prostate cancer in their family, especially if it was a first-degree relative such as a father or brother, are at an increased risk. This risk may be two to three times greater than the risk for men without a family history of the disease. Earlier age at diagnosis (<60 years of age) in a first-degree relative and disease affecting more than one relative also increases the risk for developing prostate cancer.
• Infection: Recent evidence has suggested the role of sexually transmitted infections as one of the causative factors for prostate cancer. People who have had sexually transmitted infections are reported as having 1.4 times greater chance of developing the disease as compared to the general population. • Diet: A diet high in fat has been associated with an increased risk of prostate cancer. There is also some evidence to suggest that obesity leads to an increased risk of having more aggressive, larger prostate cancer, which results in a poorer outcome after treatment.
• Chemical agents: Exposure to chemicals such as cadmium has been implicated in the development of prostate cancer.
• Hormones: Hormonal causes have also been postulated. Since Androgen ablation causes a regression of prostate cancer. In addition, eunuchs do not develop adenocarcinoma of the prostate.
Pathophysiology
The prostate is a zinc accumulating, citrate producing organ. The protein ZIP1 is responsible for the active transport of zinc into prostate cells. One of zinc's important roles is to change the metabolism of the cell in order to produce citrate, an important component of semen. The process of zinc accumulation, alteration of metabolism, and citrate production is energy inefficient, and prostate cells sacrifice enormous amounts of energy (ATP) in order to accomplish this task. Prostate cancer cells are generally devoid of zinc. This allows prostate cancer cells to save energy not making citrate, and utilize the new abundance of energy to grow and spread. The androgen receptor helps prostate cancer cells to survive and is a target for many anti cancer research studies. Prostate specific membrane antigen (PSMA) stimulates the development of prostate cancer by increasing folate levels for the cancer cells to use to survive and grow; PSMA increases available folates for use by hydrolyzing glutamated folates.
Prostate Cancer Symptoms
Most men with prostate cancer have no symptoms. This is particularly true of early prostate cancer. Most prostate cancers are discovered when a prostate biopsy is performed after a raised serum prostate specific antigen (S. PSA) blood test is noted. This test is frequently performed as a part of a health screening program. Sometimes, prostate cancers are discovered incidentally when a digital rectal exam is performed. Symptoms usually appear when the tumor causes some degree of urinary blockage at the bladder neck or the urethra.
The usual symptoms include
• difficulty in starting and stopping the urinary stream,
• increase in frequency of urination, • pain while urinating.
• The urinary stream may be diminished (urinary retention), or it may simply dribble out.
• Even after urination, there is a sense of bladder fullness because the bladder has not been fully emptied.
• Less common symptoms are hematuria, painful ejaculation, or impotence
• Men with such advanced cancers sometimes experience recurring urinary tract infections.
These symptoms, by themselves, do not confirm the presence of prostate cancer in any single individual. Indeed, most, if not all, of these can occur in men with non-cancerous (benign) enlargement of the prostate, which is the more common form of prostate enlargement as compared to cancer.
Metastatic Symptoms
Metastatic symptoms include weight loss and loss of appetite; bone pain, with or without pathologic fracture (because prostate cancer, when metastatic, has a strong predilection for bone); and lower extremity pain and edema due to obstruction of venous and lymphatic tributaries by nodal metastasis. Uremic symptoms can occur from ureteral obstruction caused by local prostate growth or retroperitoneal adenopathy secondary to nodal metastasis.
Diagnostics
The only test that can fully confirm the diagnosis of prostate cancer is a biopsy. However, prior to a biopsy, several other tools may be used to gather more information about the prostate and the urinary tract.
They include:
• Complete blood cell count: hemoglobin level and relative amounts of different blood cells are checked. Anaemia is a common sequel to cancers, as are certain other blood irregularities.
• (DRE) digit rectal examination of prostate: An irregular firm prostate or nodule is typical
• Prostatic specific antigen (PSA): Traditionally, a PSA of 4 ng/ml has been used as a cutoff value for deciding for or against doing a prostate biopsy. However, some experts now recommend lowering that to 2.5 ng/ml and performing the biopsy in men who have levels in excess of this threshold. Note that PSA may be elevated in noncancerous conditions, such as prostatitis and benign prostatic hypertrophy.
• Imaging studies: These reveal the size and location of the tumor in the prostate as well as the extent of spread of the disease.
CT scan or MRI of abdomen and pelvis: This is the best way to detect the extent of the primary cancer as well as distant metastases. Chest x-ray film: This is a simple test that shows whether cancer has spread to the lungs.
Ultrasound of kidneys, bladder, and prostate: Ultrasonography can be used to look for the effects of a urinary blockage on the kidneys. This is indicated by signs of hydronephrosis. This study can also be used to assess the bladder for any sign of urinary obstruction due to prostate enlargement by looking at the thickness of the bladder wall and the amount of urine left inside the bladder after passing urine.
Cystocopy: This may show whether the cancer has spread to the urethra or bladder.
Technetium Tc 99m bone scan: This test is like an X-ray film of the entire body taken after a mildly radioactive substance is administered into a vein. The radioactive substance highlights areas where the cancer has affected the bones. This test is usually reserved for men with prostate cancer who have deep bone pain or a fracture or who have biopsy findings and high PSA values (>10-20 ng/ml) suggestive of advanced or aggressive disease.
When the findings of the physical exam, lab tests, and imaging studies suggest that a cancer is present in the prostate, the diagnosis must be confirmed by taking a sample of the tumor (biopsy). The standard method of obtaining a prostate biopsy uses transrectal ultrasonography to guide collection of the tissue sample. The sample is collected by inserting a needle into the tumor and withdrawing cells.
Other methods of collecting samples are
1. Transuretral
2. Transvesical
3. Transperanial
A pathologist then examines the pieces under the microscope to assess the type of cancer present in the prostate and the extent of involvement of the prostate with the tumor. Another very important assessment that the pathologist makes from the specimen is the grade (Gleason's score) of the tumor. This indicates how different the cancer cells are from normal prostate tissue. Grade gives an indication of how fast a cancer is likely to grow and has very important implications on the treatment plan and the chances of cure after treatment.
Classification
Staging is a system of classifying tumors by size, location, and extent of spread, local and remote. It is an important part of treatment planning because tumors respond best to different treatments at different stages. It is also a good indicator of prognosis, or the chances of success after treatment. The stages of prostate cancer are as follows:
• Stage I (or A): The cancer cannot be felt on digital rectal exam, and there is no evidence that it has spread outside the prostate. These are often found incidentally during surgery for an enlarged prostate.
• Stage II (or B): The tumor is larger than a stage I and can be felt on digital rectal exam. There is no evidence that the cancer has spread outside the prostate. These are usually found on biopsy when a man has an elevated PSA level. • Stage III (or C): The cancer has invaded other tissues neighboring the prostate.
• Stage IV (or D): The cancer has spread to lymph nodes or to other organs.
Most doctors currently use the 2002 TNM (Tumor, Node, Metastases) staging system for prostate cancer.
T
• TX: cannot evaluate the primary tumor
• T0: no evidence of tumor
• T1: tumor present but not detectable clinically or with imaging o T1a: The tumor was incidentally found in less than 5% of prostate tissue resected (for other reasons). o T1b: The tumor was incidentally found in greater than 5% of prostate tissue resected. o T1c: The tumor was found in a needle biopsy performed due to an elevated serum PSA.
• T2: The tumor can be felt (palpated) on examination but has not spread outside the prostate.
o T2a: The tumor is in half or less than half of one of the prostate gland's two lobes.
o T2b: The tumor is in more than half of one lobe but not both. o T2c: The tumor is in both lobes. Implies a tumor which is palpable in both lobes of the prostate.
• T3: The tumor has spread through the prostatic capsule (if it is only part-way through, it is still T2).
o T3a: The tumor has spread through the capsule on one or both sides.
o T3b: The tumor has invaded one or both seminal vesicles.
• T4: The tumor has invaded other nearby structures.
N
• NX: The regional lymph nodes cannot be evaluated.
• N0: There has been no spread to the regional lymph nodes.
• N1: There has been spread to the regional lymph nodes.
M
• MX: A distant metastasis cannot be evaluated.
• M0: There is no distant metastasis.
• M1: There is distant metastasis.
o M1a: The cancer has spread to lymph nodes beyond the regional ones.
o M1b: The cancer has spread to bone.
o M1c: The cancer has spread to other sites (regardless of bone involvement).
Treatment
Treatments for prostate cancer are effective in most men. The choice of treatment depends on age, general medical condition, and the extent of the tumor spread. Approach to treatment may be conservative or surgical treatment
Conservative Treatment
• Active surveillance (watchful waiting): This consists of closely monitoring the patient's prostate cancer by performing the PSA and DRE tests regularly, and treating it only if and when the prostate cancer causes symptoms or shows signs of growing.
• Radiation therapy: There are two types of radiation therapy—
o External radiation therapy: A machine outside the body directs radiation at the cancer cells.
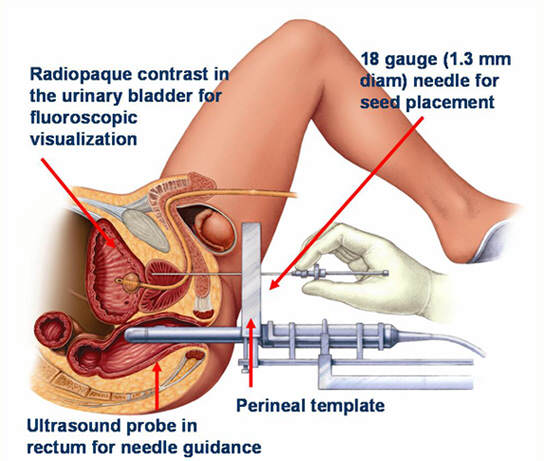
o Internal radiation therapy (brachytherapy): Radioactive seeds or pellets are surgically placed into or near the cancer to destroy the cancer cells.
• Hormone therapy: ( medical castration) This treatment uses drugs, surgery, or other hormones to remove male sex hormones or block them from working, which prevents cancer cells from growing. i.e leuprolide (Lupron, Viadur, Eligard), goserelin (Zoladex), or buserelin (Suprefact), flutamide (Eulexin) or bicalutamide (Casodex) Other therapies used in the treatment of prostate cancer that are still under investigation include—
• Cryotherapy: Placing a special probe inside or near the prostate cancer to freeze and kill the cancer cells. The long-term effectiveness of this procedure is unknown because it is a newer treatment.
• Chemotherapy: Using special drugs to shrink or kill the cancer. i.e docetaxel (Taxotere). The drugs can be pills you take or medicines given through an intravenous (IV) tube, or, sometimes, both.
• Biological therapy: This treatment works with your body's immune system to help it fight cancer or to control side effects from other cancer treatments. Side effects are how your body reacts to drugs or other treatments. Biological therapy is different from chemotherapy, which attacks cancer cells directly.
• High-intensity focused ultrasound: This therapy directs high-energy sound waves (ultrasound) at the cancer to kill cancer cells. HIFU (high intensity focused ultrasound) was first developed as a treatment of benign prostatic hyperplasia (BPH) and now is also being used as a procedure for the killing of prostate cancer cells. This procedure utilizes transrectal ultrasound that is highly focused into a small area, creating intense heat of 80 C-100 C, which is lethal to prostate cancer tissue.
Surgical Approach
• Surgery (radical prostatectomy): surgery to remove the prostate completely. Radical prostatectomy removes the prostate as well as the surrounding tissue. It may be Radical Retropubic Prostatectomy, Radical Perineal Prostatectomy or Laparoscopic Radical prostatectomy (LRP)
• Orchiectomy (surgical castration)- Men usually prefer medical castration to surgical castration. A luteinizing hormone-releasing hormone (LHRH) agonist, such as leuprolide (Lupron, Viadur, Eligard), goserelin (Zoladex), or buserelin (Suprefact), stops the production of testosterone.
• Transurethral Resection of the Prostate (TURP) –though it is not considered a standard-of-care procedure if cure is intended.
Complications/side effects of Treatment
Radiation therapy can cause impotence and/or urinary incontinence. This occurs because the radiation damages the nerve and the muscles that control these functions. These effects may be permanent, but they are less likely to be permanent with internal radiation.
Orchiectomy and LHRH agonists may cause impotence, hot flashes, and loss of sexual desire. Antiandrogens may cause nausea, vomiting, diarrhea, and breast enlargement or tenderness. Any of these therapies can weaken bones.