A SILENT EPIDEMIC - OCCUPATIONAL HAZARD
- font size decrease font size increase font size
 I had my first needle stick injury barely a week after embarking on my career as a doctor. Subsequently, I Spent the few next months getting repeat blood tests to make sure I didnt convert.
I had my first needle stick injury barely a week after embarking on my career as a doctor. Subsequently, I Spent the few next months getting repeat blood tests to make sure I didnt convert.
But then, the needle stick injuries just didn't stop there, I even got blood splashed all over my face/eyes while scrubbed in. Pretty much thought that I was going to die. It doesn't matter what the statistics are, if you get stuck with a needle or blood splatters onto your eyes, there is that moment of unbridled nausea and terror that is unexplainable.
its only a matter of time and luck
Health professionals are frequently stuck by needles, but many don’t bother reporting the injuries.
"even when you're being careful, even when you think you are too brilliant of a person to ever get stuck."
It's estimated that approximately 10,000 such percutaneous injuries occur each year. These injuries expose health care workers not only to HIV, but also to other blood-borne pathogens, such as hepatitis B and C, gonorrhea, typhus, herpes and syphilis. Approximately 500 health care workers experience infections from accidental needlesticks every year, and nearly two thirds of health workers report being stuck at some point in their career.
Less is known about needle injury rates among medical and nursing students, who, because of a lack of experience and skill, are believed to be at particularly high risk. Injections, intravenous lines, biopsies and the sewing up of incisions are mundane tasks often relegated to medical and nursing students, who typically have less experience and skill at handling needles. But when students do get pricked by a needle, they are often being graded on their overall performance, giving them less incentive to report the injury.
Most needlestick injuries do not involve HIV-infected blood. It is estimated that of the 10,000 injuries each year, only about 10 percent involve needles that are likely to be contaminated with HIV. Of those 10 percent of needlestick injuries where HIV-infected blood is known to be present, the chance of HIV transmission is estimated to be 0.45 percent. The risk of transmission may be increased, however, if the needle is visibly bloody, if the procedure involved placing the needle in one of the patient's veins or arteries, or if there was a deep injury.
Risks for HIV are small... risks for hep C, not so small.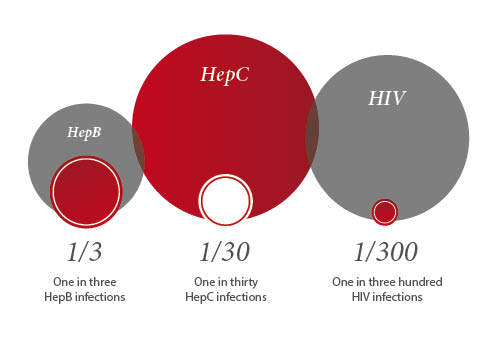
HBV - 30%
HCV - 3%
HIV 0.3%
Rule of 3s...
Regardless of the statistics, getting tested for HIV and other blood-borne pathogens can tell you for sure whether or not you've been infected.
Here’s what you can do if you’re a health care worker who has been stuck by a needle:
- *Wash the site immediately with soap and hot water.
- *Contact your supervisor for support and proper documentation of the incident.
"It is paramount to always go to health services, even if you choose not to take meds. For your own protection, you need it documented."
- *Have the source patient tested for HIV and hepatitis B and C if you’re unsure about potential infections or if the patient’s medical records are incomplete. If the patient does not consent to testing, get tested immediately and again after six months have passed.
- *Consider beginning a regimen of post-exposure prophylaxis (PEP) as soon as possible after the prick.
>>>>>>> PEP for HIV: Health care workers usually take zidovudine (AZT) or lamivudine (3TC) within the first two hours after exposure. PEP has the ability to reduce HIV contraction by up to 80%, but approximately half of health care workers on HIV PEP stop treatment early due to negative side effects. Early termination of PEP treatment may considerably reduce the efficacy of this method of infection prevention.
>>>>>>> PEP for hepatitis B: If you’re vaccinated for hepatitis B, PEP is not necessary. If you’re not vaccinated, however, the hepatitis B Immune Globulin (HBIG) injection provides short-term immunity to hepatitis B. Further, initiation of the hepatitis B vaccination series is highly recommended. Hepatitis B PEP is known to reduce infection by approximately 75 percent. If you’re unvaccinated and do not undergo PEP, your risk of transmission is between 6 – 30 percent.
>>>>>> PEP for hepatitis C: there is no standard PEP procedure for hepatitis C exposure, but inquire with your supervisor and doctor about experimental hepatitis C PEP. Hepatitis C is a serious concern, but probability of infection via needlestick injury is situated between 0 – 7%, so your chances of infection are relatively slim.
- *Receive follow-up counseling and ongoing post-exposure treatment until you and your doctor have completed all steps necessary to prevent or treat needlestick infection.
The best way to prevent these types of infections is to learn how to stop needlesticks from happening in the first place. For example, many health care facilities now use safety syringes, which can prevent accidental needlestick injuries among health care professionals by up to 80 percent.Some hospitals, have pioneered “sharpless surgery” practices that virtually eliminate the need for handling sharp objects during surgical procedures. Surgeons use lasers for cutting, glue for closing skin, minimally invasive ports for laparoscopic procedures and blunt tip needles that lower the risk of an accidental skin prick. Hospitals also need to simplify the process by which health care workers reported such injuries and received treatment.
By adhering to health care facilities’ procedures and policies about giving injections and using syringes properly (including how and when to discard them), you can make your workplace environment safer and more productive for you and your patients.
Talk to your supervisor about specific procedures for your workplace.

