Endometriosis
- font size decrease font size increase font size
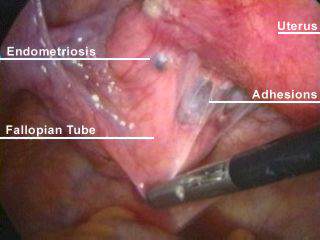
Endometriosis - a benign growth of tissue, similar in structure and function to the endometrium, but located outside the boundaries of the normal arrangement of the mucous membrane of the uterus.
Size of endometrioses ranges from microscopic up to massive tumor of endometrioid cyst, leading to marked anatomical disturbances of the uterine tubes and ovaries, as well as the formation of extensive adhesions, often damaging the bowel, bladder and ureter.
One of the special features of endometriosis is the ability of infiltrative growth with penetration into the surrounding tissue and destruction of the latter. That is why endometriosis can "grow into" any tissue or organ: the rectal wall, bladder, ureter, peritoneum, bone tissue.
Distribution
In the scheme of gynecological pathologies, endometriosis ranks third among diseases of female genital organs (after inflammation and uterine fibroids). According to VP Baskakov et al. (1998), it occurs in 17% of young patients who suffer from algodysmenorrhea, and reaches 30% in patients in need of gynecological operations. According to reference data, in the U.S. endometriosis detected in approximately 7% of women of reproductive age with abdominal pain and infertility.
Etiology and pathogenesis of endometriosis
reasons for development endometriosis up to now is not accurately established.There are several theories of the development of endometriosis, but none of them explains all aspects of the pathogenesis of this disease.
1. Translocation of the endometrium from the uterus through the fallopian tube to the peritoneum.
2. Violation of embryogenesis with abnormal residues of the Müllerian duct.
3. Metaplasia of the epithelium (peritoneum) - transformation into endometrioidnopodobnuyu tissue mesothelium of peritoneum and pleura, the endothelium of lymphatic vessels, epithelial tubules of the kidneys, etc.
4. Translocation of the endometrium of the uterus to the peritoneum and other organs at various gynecological operations (abortion, diagnostic curettage of the mucous membrane of the uterine cavity, diathermy coagulation of the cervix, cesarean section, myomectomy with the opening of the uterus, etc.).
5. Dissemination of endometrial tissue from the uterus through the blood or lymphatic vessels.
6. Violation of hormonal regulation in the system of hypothalamus, pituitary, ovaries and target organs. Violations of the cyclic production of releasing factors of the hypothalamus and gonadotropic hormones of the anterior pituitary leads to the development of absolute or relative hyperoestrogenic state and inadequate production of progesterone by the corpus luteum. Functional disability of the system of hypothalamus, pituitary, ovaries also affects the synthesis and activity of proteins and enzymes, nucleoproteins, modified antigenic properties of blood, which in turn leads to immune deficiency and promotes the development of the underlying disease.
7. The development of endometriosis as a genetically caused disease.
Pathogenesis of endometriosis appears to be highly complex and far from being solved. In the process of development of disease specific significance of the different pathogenetic factors may vary. The study of the pathogenesis of endometriosis can improve treatment and prevention of this disease.
Classification of endometriosis
Depending on the localization of endometrioid heterotopias endometriosis divided into genital and extragenital. Genital endometriosis - can be localized in the myometrium (adenomyosis) and the peritoneum, ovaries, in Douglas' pouch, rectovaginal septum, cervix, vagina and perineum.
Extragenital endometriosis topographically not associated with the tissues and organs of the reproductive system and includes the abdominal organs (appendix, rectum, sigmoid and colon, small intestine, sac), the lungs and pleural cavity, skin (episiotomy and other post-surgical scars), inguinal region , legs, navel, lymph nodes, nerves and brain.
It is widely used in international practice is proposed in 1979 and revised in 1985 and 1986 classification of the American Society of Fertility (R - AFS). It is based on counting the number of heterotopias, expressed in points: the presence of 1 - 5 centers considered to be mild, 6 -15 - to moderate, 16 - 30 - to severe, over 30 endometriosis - the widespread endometriosis. This classification was actually designed in such a way that based on the amount of points to predict the restoration of fertility after a treatment. Despite the fact that, at present being developed classifications that include the parameters of disease activity, but the revised classification of the American Society of fertility is the only internationally recognized standard for assessing the spontaneous evolution and comparison of therapeutic results.
In 1984, K. Semm, using the results of diagnostic laparoscopy, offered to provide the so-called minor forms of endometriosis. The advantage of the latter consists in the fact that this version of the spread of endometriosis is easy to identify "at first glance" at the time of laparoscopy. The concept of "small forms" external endometriosis includes endometrioid heterotopes not exceeding 0.5 cm in diameter and are usually not accompanied by marked clinical manifestations, except for infertility.
According to LV Adamian, VI Kulakov (1998), the main shortcoming of the classification of the American Society of Fertility (R - AFS) is it is limited to only the visual assessment of anatomic lesions without infiltrative forms in lesions of the rectovaginal tissue and the parameters of the functional changes clinical picture, etc.
In the daily work of widely used clinical classification of internal endometriosis (adenomyosis)of the uterine body, endometrioid ovarian cysts and retrocervical endometriosis (retrovaginal partitioning), while providing 4 stages spread of endometrioid heterotopias of the above locations. Adenomyosis is subdivided into diffuse and focal.
Classification of internal endometriosis, depending on the depth of damage is divisible by 4 degrees.
1 st degree - extension to submucosal layer;
2-nd degree - to the middle of the myometrium;
3rd degree - the entire thickness of the myometrium to serous cover;
4-th degree - involves the serous layer.
extragenital endometriosis includes; endometriosis of the bladder, bowel, postoperative scar on the anterior abdominal wall, kidneys, lungs, conjunctiva, etc.
Clinical manifestations
Clinical manifestations of endometriosis are due to the localization and degree of prevalence. One of the main symptoms of endometriosis is a progressive pain syndrome, expressed in premenstrual period and during menstruation.
Genital endometriosis causes a disturbance of the menstrual and generative functions, as well as the functions of neighboring organs - intestines and urinary tract. Disorder of menstrual function is manifested in the form of hyperpolymenorrhoea menorrhagia and menometrorrhagia and occurs usually in patients with endometriosis of the uterus.
Heavy uterine bleeding, persistent, poorly amenable to symptomatic treatment and often lead to the development of anemia. Changing the metabolism of sex hormones adversely affect the functions of hemopoeisis blood, contributes to this.
The frequency of infertility in endometriosis, according to different authors, ranging from 30-40 to 60-80%. Often endometriosis found in women subjected to laparotomy due to infertility. Infertility in endometriosis due to various reasons: the localization of endometriosis in the uterine tube angles, a violation of transport and implantation of the ovum as a result of prolonged bleeding in internal endometriosis, concomitant inflammation, inadequate luteal phase and anovulation.
Endometriosis of the uterus (adenomyosis - internal endometriosis) - one of the most frequent types of endometriosis. The main symptom is algodysmenorrhea (combination of local pain and general state disturbances). There are nodular and diffuse forms of adenomyosis. Pain depends on the form of adenomyosis, the depth of ingrowth(infiltration) in the myometrium, the peritoneal involvement in the process of endometriosis and the proximity of the sacro-uterine ligaments. Pain is more pronounced in nodular form. If we talk about the depth of ingrowth in the myometrium, the pain more pronounced if the lesion is superficial or very deep, ie characteristic of internal endometriosis I and IV degrees.
Pain is especially severe in the damage to isthmus of the uterus, sacro-uterine ligaments. Pains are radiating in nature. In injury to the angles of uterine pain radiates to the corresponding inguinal region, in endometriosis in the posterior part of the isthmus of the uterus –it radiates to the rectum.
The next most important symptom of adenomyosis - heavy, prolonged menstrual nature of menorrhagia, but can occur and metrorrhagia. Uterine bleeding is more pronounced in diffuse adenomyosis. Particularly important to note is the frequent combination of adenomyosis with uterine myoma. According to many authors the percentage of combinations ranging from 60 to 80%, with symptoms of both diseases detected. Combination fibroids and adenomyosis are often expressed pain syndrome, hyperpolymenorrhea and secondary anemia.
Endometriosis of the ovaries is the first in the group of external genital endometriosis. It should be noted that it is important not only the frequency of the disease, but also the role of ovarian endometriosis in the generalization process. Almost always injury to the intestine, diaphragm with perforation in the direction of the pleural cavity, the development retrocervical endometriosis, ureteral lesion begins with the ovaries. According to the direction of development, there are several types of ovarian endometriosis: the growing (proliferating), stable (fibrous), regressive (degenerative) and malignant.
Endometriosis of the ovaries may be asymptomatic until a given time, before the onset of microperforation of the ovarian capsule and involvement in the process of peritoneum or adjacent pelvic organs. During menstruation pain intensified. In 60-70% of patients seen algomenorrhea. When there is a perforation of the cyst picture of acute abdomen.
Any forms of endometriosis of the ovary often cause anovulatory cycles, infertility.
Retrotcervical endometriosis (endometriosis of the rectovaginal septum) may be primary, most often after diathermocoagulation or secondary in cases where the transition process in this region with adenomyosis, endometriosis of the ovaries and tubes. With this localization of foci of endometrial heterotopy spreads to sacrouterine ligaments, rectum, parametrium, posterior fornix of the vagina, ureters. The pain syndrome is expressed intensely, particularly when menstruating. Report pain during intercourse, dysureic phenomenon, bloating, constipation, irradiation of pain to lower back, coccyx, rectum.
Endometriosis tubes and vagina are extremely rare. Most tube endometriosis is found during the operation. Diagnosis is difficult. Vaginal endometriosis is determined by palpation, and visualization of growth of vaginal wall, painful swellings with indistinct borders and characteristic cyanotic areas "eyes".
The main complaint in vaginal endometriosis is the vaginal pain in the vagina and in the depth of the pelvis, from moderate to very severe. Pains are cyclical in nature. They increase with sexual life, a week before and after menstruation. Pain in the vagina may be accompanied by local itching, there may be bloody and brown discharge from the vagina. This discharge appeared a week before and after menstruation.
Endometriosis of the cervix - diagnosis is established during the inspection of the cervix, confirmed by colposcopic and histological study. There are superficial (ektotservikalny) and deep (endocervical) endometriosis of the cervix. Typical complaints are up to - and postmenstrual brown or bloody discharge or spontaneous nature of the contact. Ektotservikalny endometriosis responds poorly to hormone therapy. Better justified mechanical removal of his pockets, followed by overlay thin catgut sutures on the larger wound surface.
Extragenital endometriosis - the most frequently localized in the area of the navel and the postoperative scar in the anterior abdominal wall and perineum. Develop most often after gynecological operations. Cyanotic formations are seen on the scar or the umbilicus. During menstruation they may bleed
Methods of diagnosis
To date, the diagnosis of endometriosis question poses some problems. The vast majority of patients with clinically active endometriosis timely diagnosis of this disease is possible. To do this, first of all need to remember the existence of endometriosis and that it may give one or other clinical manifestations, sometimes pronounced at different ages, beginning with the appearance of menarche (10-14 years) and 50-60 years. At younger and older ages, the diagnosis of endometriosis is particularly precarious. The importance of diagnosing the disease in these age groups is that it can reduce the incidence of advanced forms of the disease, improve treatment results, with beneficial effects on disability and rehabilitation of specific functions of women and older women can help to differentiate the cancer and avoid unnecessary radical surgery interventions.
In the diagnosis of endometriosis plays a big role focused medical history. The leading role is cyclical manifestations of the disease and the relationship of exacerbations to menstruation. When collecting medical history is necessary to pay attention to family history in the female line (painful and heavy menstrual bleeding in the mother, sisters, and transferred their gynecological diseases and surgery). Of significant value are obstetric and gynecological operations, during which are performed opening of the uterine cavity (cesarean section, husking fibromatous nodes), surgery for uterine perforation, ectopic pregnancy, etc.
Do not forget the dependence of these objective investigations on the phases of the menstrual cycle. This applies to the size of the lesions or organs. Given the variability of the complaints and the objective data, it is useful to perform a survey of patients in different phases of the menstrual cycle.
Of considerable importance are additional methods of examination:
I. Hysterosalpingography conducted with aqueous solutions of contrast agents in the 7-8th day of the menstrual cycle, since at this time sloughed functional layer of the mucosa of uterine body does not prevent the penetration of contrast medium in endometrioid tissues. The characteristic radiological feature of internal endometriosis is the presence of "contourous shadows. In order to improve the information content of the method hysterosalpingography in the diagnosis of adenomyosis at the Department of Obstetrics and Gynecology, PFUR proposed a method where a day before the study was done scraping the mucosa of the uterine cavity. This measure facilitates the penetration of aqueous contrast to all the areas of endometrioid heterotopias. As a result, informative method increased by 3 times.
II. Hysteroscopy performed on the 8-10th day of the menstrual cycle. In the presence of internal endometriosis of the fundus or side walls of the uterus endometrioid lesions are seen as a dark-red holes, from which blood oozes. During hysteroscopy is necessary to differentiate the nodular form of endometriosis from submucosal uterine myoma.
III. Colposcopy with subsequent biopsy is used to verify the diagnosis of endometriosis of the cervix.
IV. Ultrasound in recent years widespread for the diagnosis of endometriosis. It should be noted that this method does not reveal the surface implants on the peritoneum, however, provides a reliable diagnosis of adenomyosis, endometriotic cysts, and also allows the suspected location of this pathological process in the rectovaginal septum.
This study for suspected internal endometriosis should be implemented in the second phase of the menstrual cycle -a few days before menstruation. The greatest attention, especially for diagnosing the early stages of endometriosis, should be paid to the state of the basal layer of the endometrium. Preference should be given to transvaginal ultrasound scan.
The most characteristic ultrasound signs of internal endometriosis are:
1) appearance in the myometrium of individual sections of increased echogenicity;
2) serrature and uneven thickness of the basal layer of the endometrium;
3) the preferential increase in the anterior-posterior size of the uterus and asymmetric thickening of one of its walls;
4) the presence in the zone of increased echogenicity rounded anehogennyh inclusions with a diameter of 2-5 mm, and the fluid cavities 6-33 mm in diameter, containing finely divided suspension;
5) echogenicity in the area of the leading edge of formation and reduction in long-front;
6) identification of closely spaced high and low echogenicity bands oriented perpendicular to the cavity scan.
The use of ultrasound criteria reveals internal endometriosis I st. in 88,5% of cases. However, the precise diagnosis of extent and form of the disease was possible in a much smaller number of our observations and amounted to 65,4%. Accurate diagnosis of II degree of internal propagation of endometriosis can be installed in 75% of cases, and the presence of the process - at 90%. Using transvaginal ultrasound can establish the presence of endometriosis Stage III. prevalence of 96.2%, with the focal form - 89,5%, and knots - 93,3%, and correctly to the degree of distribution - in 92,3%, 21% and 80% respectively (VN Demidov, et al. , 1997).
V. Laparoscopy - Examination of the abdominal cavity through an optical system - is carried out in the II phase of the menstrual cycle, but no later than 3-4 days before the expected menstruation. The procedure may include inspection and palpation with a blunt manipulator of the intestine, bladder, uterus, tubes, ovaries, Douglas' deepening and broad ligament. When the diagnosis of endometriosis is extremely important histological verification of the results of laparoscopy is not only barely visible areas, but even for typical homes, because, according to available data, at morfogistologicheskom study such foci in 24% of patients with symptoms of endometriosis are not available.
VI. Determining the level of CA-125.
VII. CT.
VIII. Nuclear magnetic resonance.
IX. Fibrocolonoscopy.
Treatment
For many years, virtually the only method of treatment of endometriosis is surgical. But as a rule, at a surgery removed only the visible or accessible lesions, which subsequently leads to relapse of disease. Currently, surgical removal of endometriotic foci by three conventional access: by laparotomy, laparoscopic, vaginal access or a combination of the latter with the above methods.
Modern approach to treatment of patients with endometriosis is a combination of surgical techniques aimed at maximizing removal of endometriotic foci, and hormonal therapy. Since it is known that estrogens stimulate the development of endometriosis, hormonal therapy aimed at suppressing the synthesis of estrogens. Therefore, different therapeutic measures are used in the treatment of endometriosis, all having the same goal - suppression of the hypothalamic-pituitary-ovarian system and the development of atrophic changes in the tissue of endometrioid heterotopias. Such events can be termed the establishment of the state of so-called false pregnancy (pseudopregnant) through the use of combined estrogen - gestagen drugs or active antiestrogens (derivatives norsteroidov, danazol) or agonists of LH - psevdomenopauzy. It should be recalled that psevdomenopauza not reproduce the exact state of the natural menopause. The latter is known to be characterized by low estrogen and high concentrations of gonadotropins. At the same time as when drug psevdomenopauze suppressed ovarian production of estrogen by reducing emissions in the pituitary gonadotropins, ie gipogonadotropny induced hypogonadism, or so-called pharmaceutical hypophysectomy.
Used previously diethylstilbestrol, methyl testosterone and other androgens are not currently recommended because they are not sufficiently effective and have serious side effects and have a teratogenic effect in the case of pregnancy during the period of drug therapy.
Selection of drugs and methods of their use depends on patient age, location and extent of endometriosis, and tolerability of medications, presence of concomitant gynecologic and somatic pathology (Table 1).
Modern drugs for the treatment of endometriosis
Danazol (Danazol, danoval) Dunawley Capsules 400 mg daily for 6 months in the continuous mode.
Nemestran (Gestrinone) capsules 2.5 mg 2 times a week 6 months in the continuous mode.
Nafarelin (Sinarel - U.S.) endonasal spray 400 mg / day 6 months in the continuous. mode
Zoladex 3.6 mg sc 1 time for 28 days № 3-6
Medrox progesterone-Provera - 10 mg 3 times daily for 3 months.
In the 80's, the most widely used for treating patients with endometriosis found danazol. Although modern studies have shown that danazol does not eliminate the disease, but only suppresses it, rather than to provide prevention of recurrences. Of the group antigestagens great importance of such a drug as gestrinone. He has antiprogestogennymi, antiandrogenic, antigonadotropnymi, and thus antiestrogens properties. According to many authors of the pain syndrome, including dysmenorrhea and dyspareunia or disappear by the second month of treatment, 55-60% of patients, and after 4 months of treatment - from 75-100%. Particularly good treatment effect achieved in patients who used the combined method.
Gestrinone (nemestran) is a derivative of 19-nortestosterona and possesses both androgenic, progestogenic, and antiestrogens antiprogestagenovym properties. The advantage of gestrinone yavletsya long half-life (28 days) after oral as well as the fact that the effective weekly dose of 140 times lower than that of danazol. The standard dose is 2.5 mg (in some cases, 5 mg) 2 times a week. As shown by studies in recent years, receiving 1.25 mg twice a week is just as effective. Duration of treatment is 3 - 6 months. The frequency of pregnancy after use gestrinone is 30 - 57%. Recurrence of pain is noted in 57% of patients after 18-24 months after treatment.
Currently popular are the analogs of the GnRh. One of the preparations of this group is zoladeks (at 3.6 mg 1 time n / a 26 days for 3-6 months.).
GnRh -agonists have no adverse effects on blood lipid profile, the activation of intravascular coagulation, do not have the masculinizing effect and do not lead to an increase in body weight. The side effects include hypoestrogenemia effect, hence the "flushing" the heat, excessive sweating, nervousness, depression, vaginal dryness, reduced libido and appearing in 6 months or more therapy - osteoporosis. How, generally, these phenomena do not require discontinuation of treatment. In cases of detection of loss of bone density effective combined additionally return (add-back) mode, based on the principle of restoring estrogen levels (use of natural estrogens).
The rate of pregnancy ranged from 24 - 52%, relapse of symptoms in 4 - 12 months. after treatment of GnRH analogues appear in 15 - 20% of patients.
Differential diagnosis
Endometriosis, depending on its localization necessary to differentiate the various diseases of the genital organs.
Endometriosis of the uterus (adenomyosis) usually have to differentiate with uterine myoma (usually with a submucous myoma node). In the presence of submucous myomas menses become erratic, acyclic, ie acquire the character of metrorrhagia. For endometriosis is characterized by menorrhagia. In submucous myoma anemia, as a rule is stable and growing depending on the blood loss. In adenomyosis anemia after menstruation relatively quickly eliminated. In terms of diagnosis used methods such as hysterosalpingography and hysteroscopy.
To differentiate this disease from cancer of the endometrium, use a separate diagnostic curettage of the cervical mucus and mucosa of the uterine cavity with subsequent histological examination.
Endometriosis of the ovaries must be differentiated from tumor-like formation of an inflammatory nature, benign and malignant tumors, tuberculosis, uterine appendages.
Endometriosis of the cervix differentiate diseases such as cervical erosion, endocervicitis, erythroplakia, cancer of the cervix.
Retrotcervical endometriosis is characterized by slow growth endometrioid formation, lack of propensity to decay, ulcers and bleeding tissue, as well as the presence of "bluish eyes". The differential diagnosis of retrocervical endometriosis with cancer of the rectum, vagina, cancer of the ovary III - IV stage. must be remembered that in such patients there are significant changes in the formula of the blood, often occurs ascites, attention is drawn to the general condition of the patient and other signs of cancer pathology.
Prevention of endometriosis
A significant prevalence of endometriosis and a tendency to increase the frequency of its dictate the need for prevention of the disease and prevent its recurrence.
As the leading role in the pathogenesis of endometriosis are offset and the implantation of elements of the endometrium outside the uterine cavity, with appropriate background and hormonal disturbances of immune homeostasis, the prevention measures should include these factors:
1. timely and sufficiently vigorous treatment of chronic inflammatory processes of the internal reproductive organs;
2. introduction of modern contraceptives to prevent unwanted pregnancies;
3. strict medical approach to the various diagnostic and therapeutic procedures (diagnostic curettage, hysterosalpingography, sounding the uterus, the operation from opening the uterus, cesarean section, etc.);
4. treatment of uterine bleeding with the use of hormones after scraping the mucosa of the uterine cavity;
5. injury prevention of the birth canal (careful suturing ruptures of the cervix, the walls of the vagina, perineum);
6. prevention of the disease after diathermocoagulation and diathermoconization cervix;
7. timely identification and correction of metabolism of sex hormones.
