SILENT NO MORE: GET HELP FOR YOUR HEMORRHOIDS/PILES
- font size decrease font size increase font size
 Hemorrhoids are horrible, discomforting and can be a painful recurrent bother. They are one of the most common ailments known. Statistically speaking,
Hemorrhoids are horrible, discomforting and can be a painful recurrent bother. They are one of the most common ailments known. Statistically speaking, more than half the population develops hemorrhoids, usually after age 30. A majority of people suffer in silence for a long period before seeking medical care.
Hemorrhoids are vascular structures in the anal canal which act as a cushion thus helping in stool control. During defecation pressure builds on the rectal veins, which sometimes causes them to bulge. As a result the tissues supporting the vessels stretch causing the vessels to dilate. With time their walls become thin and bleed and if the stretching and pressure continues, the weakened vessels protrude.
The cause of excessive pressure and weakening of the walls may be due to:
• Chronic constipation or diarrhea
• Pregnancy
• Straining during bowel movements
• Faulty bowel function due to overuse of laxatives or enemas
• Spending long periods of time in the toilet
These swollen blood vessels can turn bowel movements into intensely painful experiences. Classic symptoms include rectal pain, itching, bleeding, and possibly protrusion of hemorrhoids into the anal canal.
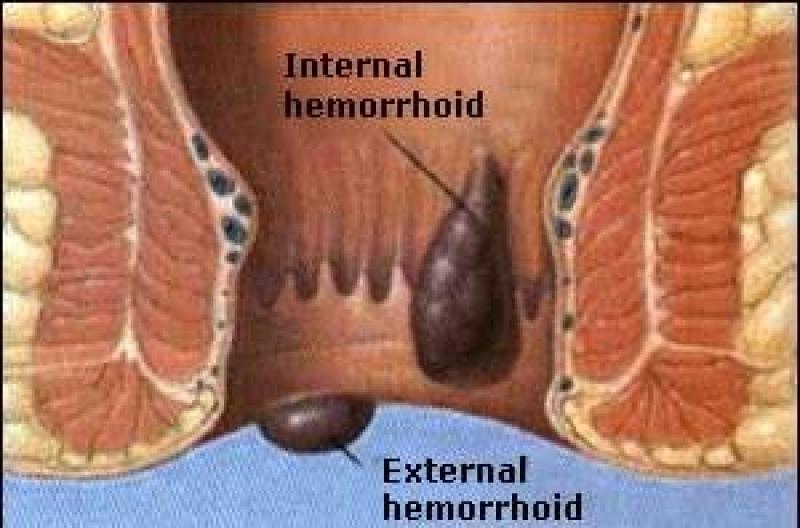
Hemorrhoids, "varicose veins of the anus and rectum", can be external or internal in reference to their location.
External hemorrhoids develop near the anus and are covered by very sensitive skin. They are usually painless but can become hard and painful if a blood clot develops in the external hemorrhoid. Sometimes they even rupture and bleed.
Internal hemorrhoids develop within the anus beneath the lining. Painless bleeding and protrusion during bowel movements are the most common symptom. Internal hemorrhoids can cause severe pain if it completely protrudes from the anal opening and cannot be pushed back inside.
Haemorrhoids often settle down after a few days without treatment. However, a number of simple self-help measures can ease the ordeal.
EFFECTIVE STEPS YOU CAN TAKE TO CARE FOR HEMORRHOIDS
1. Step up the fiber.
The most important thing is to add fiber to your diet. Fiber helps you avoid constipation and straining to pass a bowel movement, which are both primary risk factors for developing hemorrhoids. A high-fiber diet also reduces the pain of hemorrhoids by making the stool soft and easier to pass. The recommended amount is 14 g of fiber per 1000 calories, or 25 g/day for a woman and 38 g/day for a man. High fiber foods include fruits, vegetables, beans, bran, and whole-grain cereals and breads.
Some people find they need to take a fiber supplement to get 20 to 30 grams of fiber per day. You can use a psyllium husk fiber supplement or wheat dextrin which can be purchased without a prescription at a pharmacy/chemist.
2. sitz bath
Water can be very soothing to inflamed and painful hemorrhoids. Applying cold compresses or using a basin that fits under the toilet seat to soak your rectal area in warm water for about 10 minutes several times a day can offer relief.
Wiping gently with moist towelettes, instead of toilet paper, is beneficial and convenient.
3. Act on the Urge
Don’t wait for a more convenient time. Delaying defecation can lead to constipation as well as aggravate and encourage the development of hemorrhoids.
4. Off-the-shelf remedies.
Over-the-counter products offer quick relief of hemorrhoid symptoms. These include hemorrhoid creams, gels, foams, suppositories, and pads that contain hydrocortisone, witch hazel, or a constricting or numbing medication such as, Preparation H and its generic equivalents. Oral medications that can help reduce inflammation and pain include acetaminophen, aspirin, and ibuprofen.
5. Stay Hydrated
Water is key to producing soft stool. Drinking enough water will not only ease the pain but can also help prevent hemorrhoids. You should drink about eight 8 glasses of water a day. Drink more in hot weather and during exercise.
Avoid or limit alcohol and caffeine intake as they promote the loss of water from your body, hence the hard stools and increase in pain of hemorrhoids.
6. Include in Diet
Mix a tablespoon of mineral oil with applesauce or yogurt and eat it at breakfast or lunch . This allows stool to slide by the hemorrhoid more easily. But don’t do this for a long period. If you try this, you may want to place a liner in your undergarments to absorb any oil leakage.
7. Exercise
A great way to ease your hemorrhoid problems is to lose weight. The excess weight around your abdomen and waist areas increase the pressure put on the veins in and around the anus. If your daily life or job includes sitting for long periods of time, be sure to get up and move around for a few minutes every hour or so.
However, certain physical activities should be avoided, including heavy lifting and anal intercourse, all of which can increase the risk of hemorrhoids and worsen symptoms.
8. During pregancy
Lying on your left side when resting or sleeping can help reduce pressure on certain veins that lead to vein swelling and hemorrhoids.
9. Try elevation
Elevating your feet a bit with a step stool as you sit on the toilet changes the position of the rectum in a way that may allow easier passage of stools.
WHEN SHOULD I CONSULT MY DOCTOR?
If the self care tips fail, hemorrhoids begin to bleed, interfere with bowel movements, or make life difficult, consult your doctor on medical procedures to remove or reduce hemorrhoids.
WHAT HAPPENS AT THE DOCTORS?
First, your health care provider will conduct a rectal exam. He/she may insert a lubricated gloved finger, an anoscope or a proctoscope.
If indicated more procedures can be conducted to identify internal hemorrhoids and rule out other ailments such as anal fissure, colitis, Crohn's disease, and colorectal cancer. These include; sigmoidoscopy or the entire colon may be viewed with colonoscopy, barium X-ray can also show the outline of the entire colon's interior.
For mild cases the doctor may then recommend certain measures that will decrease the pain and swelling of most symptomatic hemorrhoids, in two to seven days. Your physician may elect to remove the hemorrhoid containing the clot with a small incision, a simple outpatient procedure performed under local anesthesia.
Severe hemorrhoids may require special treatment. Your doctor may suggest one of the following procedures
1. Injection.
Internal hemorrhoids can be injected with a solution which creates a scar and closes off the hemorrhoid.
2. Banding/Ligation
Prolapsed hemorrhoids are often removed using this procedure. A special tool secures a tiny rubber band around the hemorrhoid, shutting off its blood supply almost instantly. Within a week, the hemorrhoid shrivels and falls off.
3. Coagulation or cauterization
By using either an electric probe, a laser beam, or an infrared light, a tiny burn painlessly seals the end of the hemorrhoid, causing it to close off and shrink.
4. Surgery/Hemorrhoidectomy
Large internal hemorrhoids or extremely uncomfortable external hemorrhoids are usually surgically removed.
Note that although hemorrhoid removal treatments are very effective, hemorrhoids may recur, unless dietary and lifestyle changes are made
Tagged under :