There are so many different types of contraception out there. Choosing the method of contraception that is right for you requires accurate information and the ability to communicate openly with your partner. Issues such as effectiveness, safety and adverse effects need to be weighed against convenience, cost and issues of trust and control.
A Contraception may be temporary or permanent. Contraceptives available include:

>abstinence during fertile phase
-
- >withdrawal also known as coitus interruptus
> cervical cap, diaphragm
> hormonal pills that alter cervical mucus thus prevent entry of sperms
3. -intra uterine devices (IUDs)
4. -hormonal contraceptives that suppress ovulation
5. -postcoital contraception- after sex pills
6. -surgical sterilization
This article shall highlight the pros and cons of each contraceptive method and how these methods meet your current and future needs. Before we embark on that, let me start by stating that, a good contraceptive method should be
- coital independent
- affordable and readily available
- have very minimal or no side effects
- long acting
- reversible -fertility returns on discontinuation
These methods have the highest failure rate and are least recommended. The failure rate of a contraceptive method is described in terms of pregnancy rate per 100 woman years (the pearl index)
A) abstinence during the fertile phase {30 per 100 women}
The fertile phase of the menstrual cycle can be determined using:
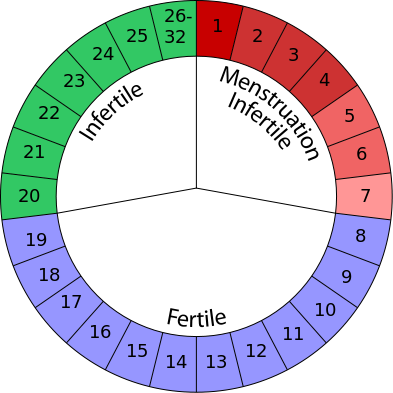
1. Rhythm method
The safe period is calculated from the first day of menstrual period until the 10th day of the cycle and from the 18th to 28th day. Therefore the risk period, when one should abstain from sex is three days before ovulation to three days after ovulation. 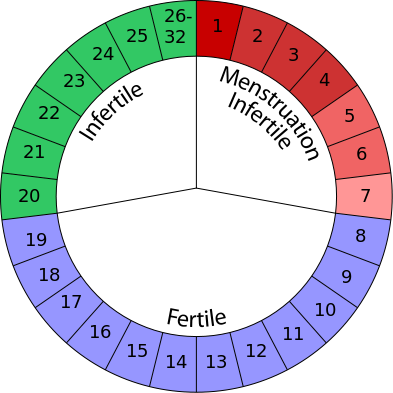
In a 28 day cycle, ovulation may occur between the 12th and 16th day. The ovum released lives for 12 to 24hrs. Therefore, intercourse between the 11th and 17th day may result in a pregnancy.
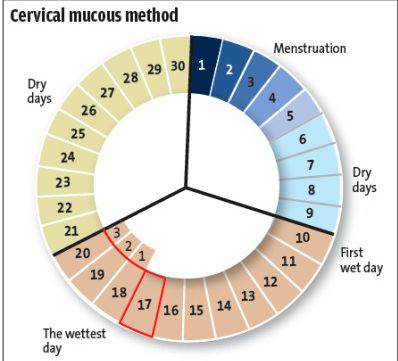
2. Mucus method
Under the influence of ovarian hormones, the properties of cervical mucus vary on different days of the menstrual cycle. Under oestrogen influence, the mucus i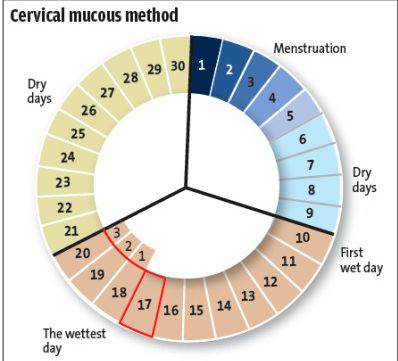 ncreases in quantity becoming more slippery and elastic. Whereas under the influence of progesterone, the mucus turns thicker, scanty and dry until onset of menses. Intercourse is considered safe during the 'dry days' immediately after menses. So the couple should abstain when mucus is detected.
ncreases in quantity becoming more slippery and elastic. Whereas under the influence of progesterone, the mucus turns thicker, scanty and dry until onset of menses. Intercourse is considered safe during the 'dry days' immediately after menses. So the couple should abstain when mucus is detected.
3. Basal temperature method
Every morning on awakening, you should record your basal body temperature. One then plots the readings graphically. The chart will be biphasic in an ovulatory cycle. The period of temperature shift marks the fertile period when one should desist from intercourse.
A) Coitus interruptus
A common practice, whereby the penis is withdrawn just before ejaculation. Note that the prostatic fluid secreted prior to ejaculation  contains sperms in majority of the cases, therefore this method has a high failure rate
contains sperms in majority of the cases, therefore this method has a high failure rate
Although natural methods of contraception cost nothing, have no side effect and may be prefered by couples on religious grounds, they are very unreliable, require motivation and offer no protection against HIV and STDs.
B) Barrier methods
1. Condoms {10 per 100 women}
Condoms are readily available, cheap, easy to carry, can prevent STD transmission and are free from side effects. Other advantages of using condoms are:
- reduced occurence of cancer of cervix- viral infection causing this disease is prevented
- can be used along with other methods to enhance efficiency
- has no adverse effect on pregnancy should the method fail
- can be used by lactating mothers. No negative effect on lactation ( breast milk production)
The drawbacks of this method are that:
-it's coitus dependent
- some people are allergic to the latex type
- improper use may cause it to burst or slip off
- tendency to non compliance
Note that the high failure rate is mainly due to improper use.
2. Spermicidal agents {30 per 100 women}
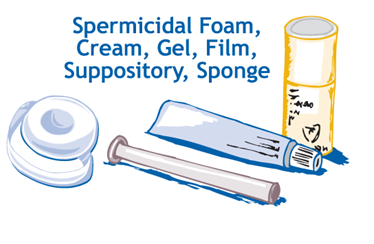 These agents kill the sperms before they gain access to the cervical canal. it is advisable to use these agents in conjuction with a mechanical barrier, i.e condom or diaphragm.
These agents kill the sperms before they gain access to the cervical canal. it is advisable to use these agents in conjuction with a mechanical barrier, i.e condom or diaphragm.
Once applied, it remains effective for 1-2 hrs.
3. Diaphragms {9-30 per 100 women}
This method is more effective when used in conjunction with a spermicide. It provides a barrier against direct insemination.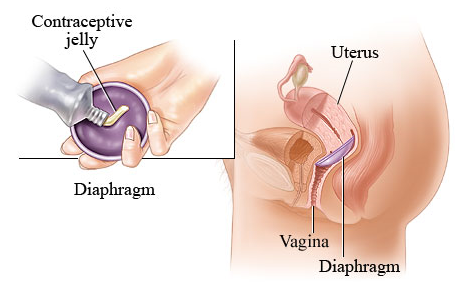
Sufficient time should be allowed for complete destruction of the sperms before its removal (left inside for a minimum of 8hrs after sex)
If you opt for this method, a routine check-up is required as alterations in size and type of diaphragm may be required due to changes in weight, illness and delivery.
Intra Uterine Devices (IUDs) {3 per 100 women}
 Most IUDs are made of polythylene and are impregnated with barium sulphate to make them visible under x-rays. Each device has a nylon thread attached to its end. This thread protudes through the cervical canal into the vagina, when the device is fitted into the uterus. The woman should feel for the thread every week to ensure the device is still in place.
Most IUDs are made of polythylene and are impregnated with barium sulphate to make them visible under x-rays. Each device has a nylon thread attached to its end. This thread protudes through the cervical canal into the vagina, when the device is fitted into the uterus. The woman should feel for the thread every week to ensure the device is still in place.
The IUDs act by:
- causing leucocytic infiltration in endometrium that engulf egg
- causing enzymatic and metabolic changes to endometrium that hinder implantation
- increasing tubal perilstalsis thus egg reaches uterus before chorionic villi is well developed to attach to wall
- rendering migration of sperms dificult, there being a foreign Body
- forming a mucus plug in cervix that blocks passage of sperm- for IUDs carrying progestagen
Examples of IUDs are Copper T, progestasert, saf-T-coil and Mirena
IUD is a long term method of contraception. It is coitus independent, has minimal negative effects and is highly effective.
The contraindications for it's use are;
- woman with heart disease= risk of vasovagal attack
- woman who has history of ectopic pregnancy= High risk of ectopic pregnancy
- levonorgestrel IUDs in breast cancer patients
- woman with fibroids
- pelvic inflammatory disease (PID)
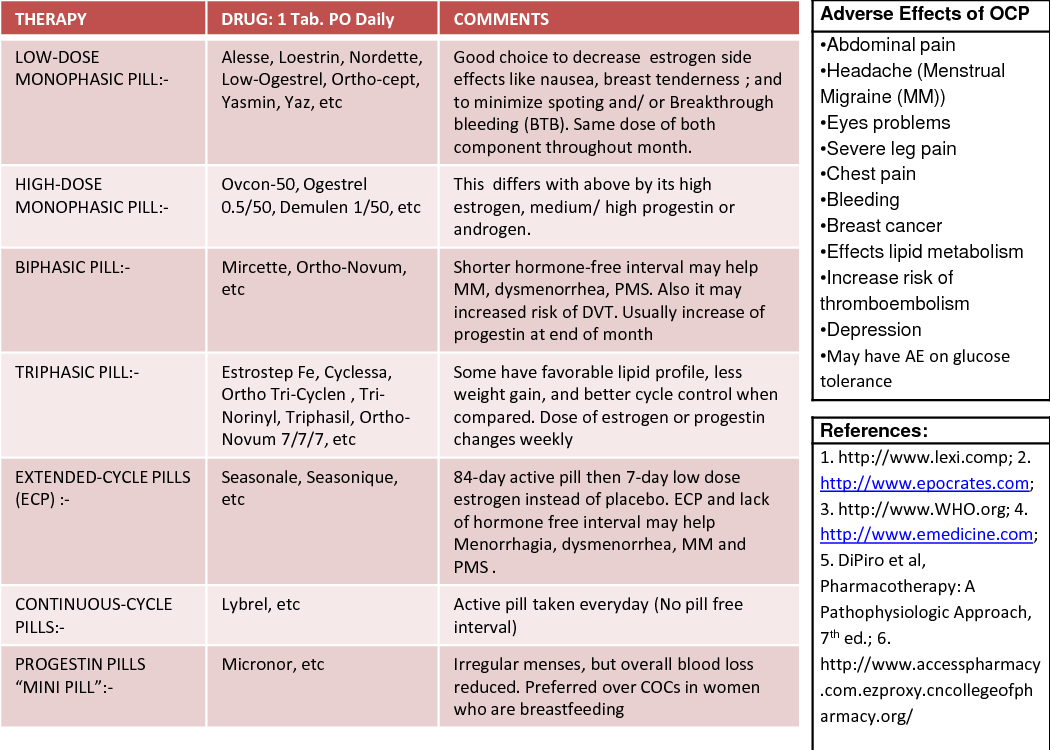
Hormonal pills
1. Pills altering cervical mucus POP { 2 per 100 women}
The minipill is administered daily. It contains progesteron, under which the cervical mucus turns thick, (cervical plug) preventing sperms from penetrating. It also supresses ovulation.
Its started on 5th day of menstuation and taken daily at the same time (leeway of 3hrs on either side of the fixed time)
If by chance you miss to take a pill on a given day, you continue taking the pill but abstain or use a barrier method within the next 48 hrs.
The pill is safe for use by lactating mothers and is usually started 21 days after delivery (postpartum).
2. Pills supressing ovulation
Combined oral pills -Biphasic {0.1 per 100 women}
The pills supress pituitary hormones, namely follicle stimulating hormone (FSH) and leutinising hormone (LH).
They are taken for 21 days from the fifth day of the cycle ( a doctor may recommend starting the pill on 1st day of cycle). They should also be taken at a fixed time everyday.
This pill causes regular scanty menstruation, therefore may be highly recommended to women experiencing heavy menses (menorrhagia) or irregular menses (polymenorrhoea). It also reduces occurence of ovarian cysts, PID, ectopic pregnancy, rheumatoid athritis and ovarian cancer.
The pill is contraindicated in persons with
- history of thrombosis( clots)
- thyroid disease
- breast cancer
- lactating mothers
- cardiac disease
- smokers over 35yrs
- hypertensive patients
- chronic liver diseases
- person on anti- epileptics
- sickle cell anemia
- uses contact lenses
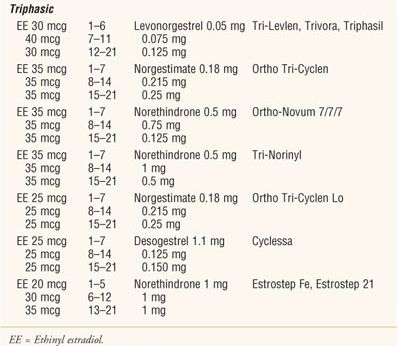
Triphasic pills {0.1 per 100 women}
These pills can be safely prescribed to diabetics. They are usually color coded and contain different quantities of ethinylestradiol and levonogestrel.
Other forms of hormonal contraceptives are: {0.2-2.8 per 100 women}
Depot injections
Subdermal implants
Vaginal rings
Skin patches
These forms elimit the failure rate of non compliance. They are long lasting, coital independent, have very low failure rate among other advantages.
Post coital contraception {0-1.6 per 100 women}
Polpularly known as plan B. These emergency contraceptives come in handy in the event of accidental rupture of condoms, rape cases or spontaneous unprotected sex. They must be taken within 72hrs following exposure.
They must not be used as a regular contraceptive technique .
They act by:
 - Causing Luteolytic effect on ovary
- Causing Luteolytic effect on ovary- Delaying ovulation
- Cause cervical mucus changes
- Cause endometrial atrophy
Note that copper T can be used as a postcoital contraceptive (emergency contraceptive) by inserting it within 5 days following exposure.
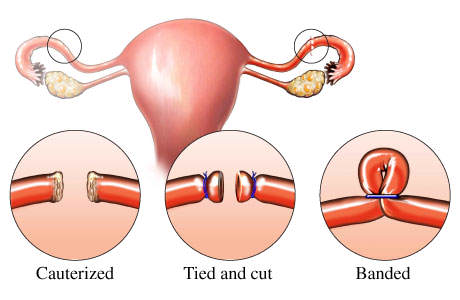
Permanent Methods
Vasectomy (male sterilization) {0.1 per 100 women}
The passage way (vas deferens) of sperms is divided. Note that after the procedure, sterility is not immediate. Other methods of contraceptives must be used until absence of sperm is confirmed.
Note that , there is a chance of recanalization after some years.
Tube ligation/cutting ( female sterilization) {0.6 per 100 women}
You may have to try several different things before you choose the one you like most. You can discuss your options with your doctor or at the reproductive health centre (family planning).
 Due to increased cost of living, scarcity of accomodation, resources and an overall desire to improve living standards, there is a pressing need to limit the family size at a personal and national level. To achieve this, we all, at one time or another, use a contraceptive method. But how do we know we're using what best suits us?
Due to increased cost of living, scarcity of accomodation, resources and an overall desire to improve living standards, there is a pressing need to limit the family size at a personal and national level. To achieve this, we all, at one time or another, use a contraceptive method. But how do we know we're using what best suits us?
 ncreases in quantity becoming more slippery and elastic. Whereas under the influence of progesterone, the mucus turns thicker, scanty and dry until onset of menses. Intercourse is considered safe during the 'dry days' immediately after menses. So the couple should abstain when mucus is detected.
ncreases in quantity becoming more slippery and elastic. Whereas under the influence of progesterone, the mucus turns thicker, scanty and dry until onset of menses. Intercourse is considered safe during the 'dry days' immediately after menses. So the couple should abstain when mucus is detected.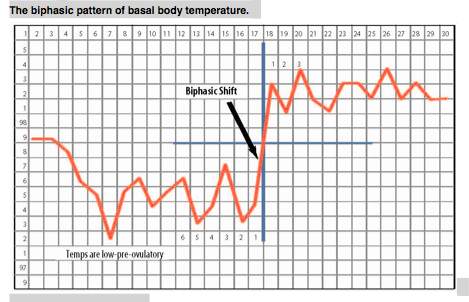
 contains sperms in majority of the cases, therefore this method has a high failure rate
contains sperms in majority of the cases, therefore this method has a high failure rate
 These agents kill the sperms before they gain access to the cervical canal. it is advisable to use these agents in conjuction with a mechanical barrier, i.e condom or diaphragm.
These agents kill the sperms before they gain access to the cervical canal. it is advisable to use these agents in conjuction with a mechanical barrier, i.e condom or diaphragm. 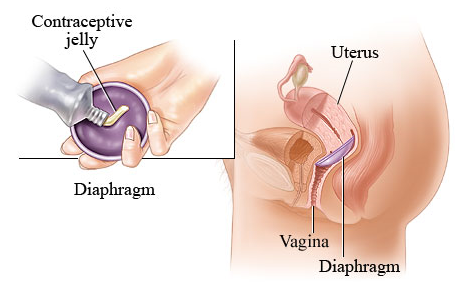
 Most IUDs are made of polythylene and are impregnated with barium sulphate to make them visible under x-rays. Each device has a nylon thread attached to its end. This thread protudes through the cervical canal into the vagina, when the device is fitted into the uterus. The woman should feel for the thread every week to ensure the device is still in place.
Most IUDs are made of polythylene and are impregnated with barium sulphate to make them visible under x-rays. Each device has a nylon thread attached to its end. This thread protudes through the cervical canal into the vagina, when the device is fitted into the uterus. The woman should feel for the thread every week to ensure the device is still in place.






 - Causing Luteolytic effect on ovary
- Causing Luteolytic effect on ovary