Laryngeal fractures
- font size decrease font size increase font size
 A traumatically injured patient may present with many distracting injuries. Appropriate treatment of this patient requires that airway patency be the first priority. Injury to the larynx may range from simple mucosal tears to fractured and comminuted cartilage. Any combination of injuries along this continuum can result in a precipitous airway emergency.
A traumatically injured patient may present with many distracting injuries. Appropriate treatment of this patient requires that airway patency be the first priority. Injury to the larynx may range from simple mucosal tears to fractured and comminuted cartilage. Any combination of injuries along this continuum can result in a precipitous airway emergency.
Laryngeal fractures can be categorized as either penetrating or blunt injuries, which can be further categorized as either high or low velocity.6Most commonly, trauma to the larynx occurs as a result of a motor vehicle accident (MVA) or clothesline injury. A small percentage of causes include direct blows sustained during assaults, sport injuries, hanging, manual strangulation, and iatrogenic causes.
The cornerstones of diagnostic evaluation in suspected laryngeal trauma are flexible laryngoscopy and computerized tomography (CT scan). Based on the physical, endoscopic and radiographic findings, these injuries can be classified into one of four groups using Schaefer's classification system:
Group 1: minor endolaryngeal edema, lacerations,
no detectable fractures
Group 2: moderate edema, lacerations
mucosal disruption without exposed cartilage
nondisplaced fractures
Group 3: massive edema, mucosal disruption
displaced fractures
cord immobility
Group 4: group 3 and
two or more fracture lines
skeletal instability
Direct trauma
Open trauma
1- Gun shot
2- Cut throat
Closed trauma
1- Mechanical: (blows, strangulation, car accidents, sport trauma, ...) etc
2- Surgical trauma: (intubation, bronchoscopy, arrytenoid subluxasion ...) etc
3- Burns & scalds: (irritant fumes, steam, corrosives, ...) etc
4- Radiotherapy
5- Foreign bodies
Indirect trauma
Psychological e.g. aphonia
Habitual voice abuse e.g. singer nodule
Diagnostic Procedures
- The procedures below are used to evaluate patients with suspected laryngeal trauma.
- Fiberoptic nasopharyngoscopy: This procedure is performed in a conscious patient, with topical anesthesia. The goal of the procedure is to evaluate vocal cord function and to perform a preliminary assessment of the extent of trauma.
- Direct laryngoscopy: This procedure provides a detailed visual examination of the larynx. Instrumentation such as the Dedo or Pilling laryngoscope provides excellent visualization; however, complete examination of the anterior commissure may require special instrumentation.
- Bronchoscopy: This procedure may be performed with either a flexible or rigid bronchoscope, depending on the experience of the operator. Examination allows observation of the subglottic larynx and supporting structures.
- Esophagoscopy: This procedure allows visualization of the esophageal mucosa for traumatic lacerations. It may be performed with either a flexible or rigid esophagoscope, depending on the experience of the operator. Traumatic injury is common in the retrolaryngeal esophagus; therefore, close evaluation is required.
Management of Traumas
Table
|
Group |
Symptoms |
Signs |
Management |
|
Group 1 |
Minor airway symptoms |
Minor hematomas |
Observation |
|
Group 2 |
Airway compromise |
Edema/hematoma |
Tracheostomy |
|
Group 3 |
Airway compromise |
Massive edema |
Tracheostomy |
|
Group 4 |
Airway compromise |
Massive edema |
Tracheostomy |
Treatment
Mucosal tears of less than 2 cm have been treated effectively without surgical intervention. Typically, in such minor injuries, tracheotomy is not required; however, close clinical observation is essential in the first 24-48 hours after injury.
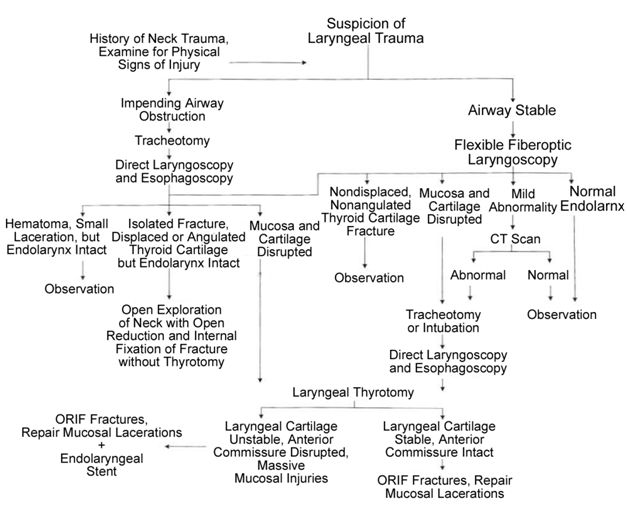
Further treatment depends on the extent of laryngeal damage. Those victims with Group 1 traumatic injuries can be treated medically with close observation, head-of-bed elevation, and humidified inspired air. Group 2 injuries usually require tracheotomy for airway stabilization and control. Direct laryngoscopy and esophagoscopy should also be performed as soon as possible. Group 2 patients can often be decannulated in three to four days. Group 3 and 4 trauma require airway stabilization followed by open exploration via a midline thyrotomy.
When open exploration is required it should be performed within the first 24 hours after the injury. Careful attention must be directed towards limited debridement of mucosa and cartilagineous fragments, meticulous closure of all mucosal defects with fine absorbable suture, and reduction and fixation of laryngeal fractures. Endolaryngeal stents may be necessary when massive mucosal disruption or comminuted laryngeal skeletal fractures are present. Stents are also required when the anterior commissure or true vocal fold margins are involved.
The keys to successful outcome in blunt laryngeal trauma are prompt, early intervention; limited debridement; and meticulous wound closure. If these principles are followed an excellent prognosis can be expected in both respiratory and phonatory ability.
Bed rest is recommended for patients treated medically for laryngeal trauma, with the head of the bed elevated 30-45°. Voice rest is recommended to minimize edema, hematoma formation, and subcutaneous emphysema. Humidified air reduces crust formation and transient ciliary dysfunction. Supplemental oxygen is usually not needed and may be harmful in some patients (eg, patients with chronic obstructive pulmonary disease).
Initially, a nothing by mouth (NPO) status is recommended for patients with laryngeal fractures and mucosal tears, followed by a clear liquid diet.13Diet regimens should mirror the severity of injury. Those patients without visible mucosal lacerations or fractures can initiate a clear liquid diet earlier than those patients with more severe injuries. Patients with severe injuries may require total parenteral nutrition supplementation during their NPO period. Avoid the use of nasogastric tubes for suctioning or feeding because of the potential for worsening laryngeal injury that results from local trauma during tube placement.
The benefit of using systemic corticosteroids is controversial. Many otolaryngologists believe that corticosteroids are necessary to retard inflammation, swelling, and fibrosis and to help prevent granulation tissue formation. Systemic corticosteroids are helpful only in the first few days after the injury.
The use of antibiotics is not necessary in the treatment of minor laryngeal trauma in which cartilaginous fractures and mucosal tears are not identified. However, when tears are visualized or with compound fractures of the larynx, systemic antibiotics should be used to reduce the high risk of local infection and perichondritis, which may delay healing and promote airway stenosis.
The use of antireflux medications, such as H2-receptor antagonists and proton pump inhibitors, can help to reduce granulation tissue formation and tracheal stenosis. Use these medications throughout the emergent and convalescent phases of medical treatment for laryngeal fractures.
Surgical Therapy
The surgical management of an unstable patient can be guided by the flow diagram depicted in the image below.
Surgical exploration begins with a horizontal skin incision in a skin crease at the level of the cricothyroid membrane. A subplatysmal apron flap is then elevated superior to the hyoid bone and inferior to expose the cricoid cartilage. Extension of the incision site facilitates examination of neural, vascular, and visceral injuries. The strap muscles are separated in the midline and are retracted laterally so that the laryngeal skeleton can be assessed adequately. At this point, identify and remove fractured pieces of the laryngeal cartilage.
Depending on the injury, the larynx is entered through the thyrohyoid membrane, a midline thyrotomy, or the thyroid cartilage within 2-3 mm of the thyroid notch. If a thyrotomy is needed, a midline, vertical perichondrial incision is made in the thyroid cartilage. A subchondral dissection follows bilaterally. An oscillating saw or a number 15 blade can be used to cut through the thyroid cartilage, with care to avoid trauma to the endolaryngeal mucosa.
After the thyroid cartilage is divided, the endolaryngeal mucosa is sharply divided. The endolarynx is examined in its entirety to identify the full extent of injury. The arytenoids are palpated to evaluate their mobility and position. Vocal cords are repaired using 5-0 or 6-0 absorbable sutures. Suturing the anterior surface of each damaged cord to the external perichondrium with 4-0 absorbable sutures resuspends the vocal cord. Reconstituting the anterior commissure is critical to preserving voice quality.
Great care should be taken to identify and repair all mucosal lacerations with fine absorbable sutures (ie, 5-0, 6-0). Primarily close exposed cartilage with meticulous technique to minimize fibrosis and prevent formation of granulation tissue. Exposed cartilage that cannot be closed primarily may need skin or mucous membrane grafts. In the few circumstances in which a graft is required, mucous membrane, dermis, or split-thickness grafts are suitable.14
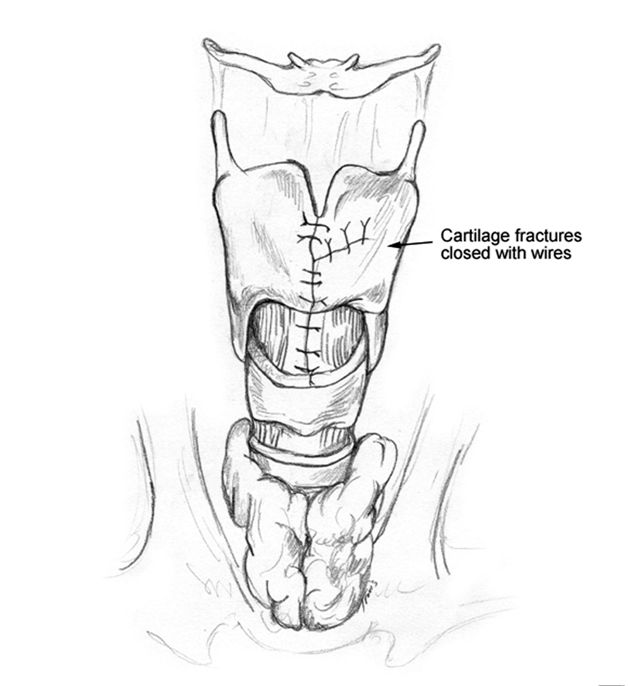
Laryngeal cartilage fractures must be reduced and immobilized. Small, isolated cartilage fractures that have no perichondrium are débrided to prevent chondritis and vocal cord dysfunction.
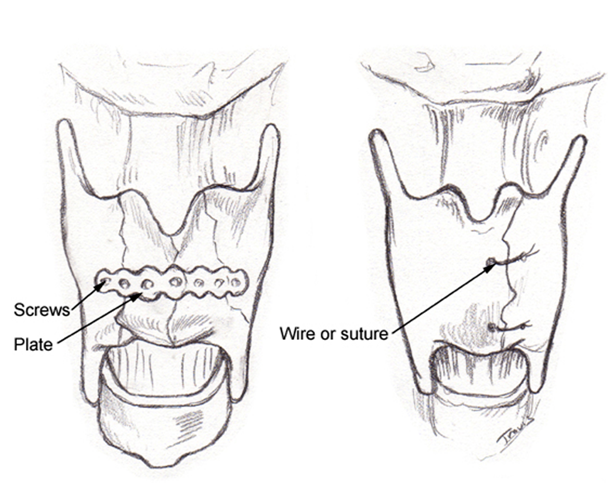
Traditionally, wire sutures have been used to immobilize reduced laryngeal cartilage fractures as seen in the image below.
Recently, however, many surgeons have begun to use metal alloy plates (miniplates) for repairing laryngeal fractures. Miniplates have been shown to effectively stabilize the laryngeal architecture as seen in the image below and reshape the larynx back to its preinjury state. They also decrease the length of hospitalization, insignificantly alter operating time, and usually add no additional discomfort to the patient.15,16The image below depicts stabilization methods.
More recently, the use of absorbable miniplates has been introduced. These plates have been found to be just as safe, effective, and manageable as their alloy counterparts. They also have the advantages of improved cosmesis after resorption, less bone growth restriction, less issue with plate migration, less bony resorption, and negligible image artifact.17Most plates are composed of polylactic acid copolymer material and used for open reduction and stabilization of displaced fractures. Sasaki et al evaluated the efficacy of both MacroPore and Leibinger restorable reconstruction plates in 3 adult male patients and found both plates to be equally easy to use. In addition, adequate skeletal stabilization was achieved, which allowed for early phonation and respiratory function without long-term stenting.18
In Brazil, de Mello-Filho et al performed a retrospective study on the efficacy of adaptation plate fixation (APF) to repair the larynx. This group had no complications with the use of APF, and 19 out of 20 patients recovered their voices.19
Regardless of the method, the goal of surgical intervention is to restore the 3 primary functions of the larynx: breathing, phonating, and swallowing.
Using permanent sutures or wires, the thyrotomy is then closed, and the strap muscles are reapproximated. The nasogastric tube is then placed using direct visualization.